|
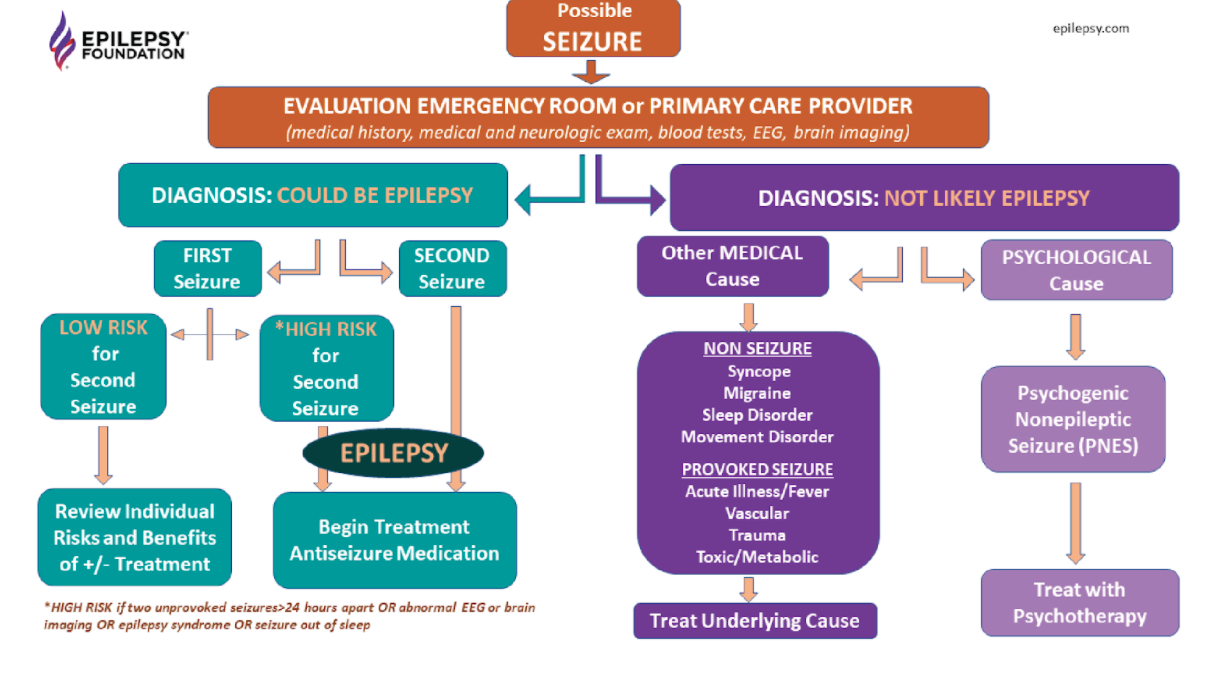
Written by Anwar Subhani 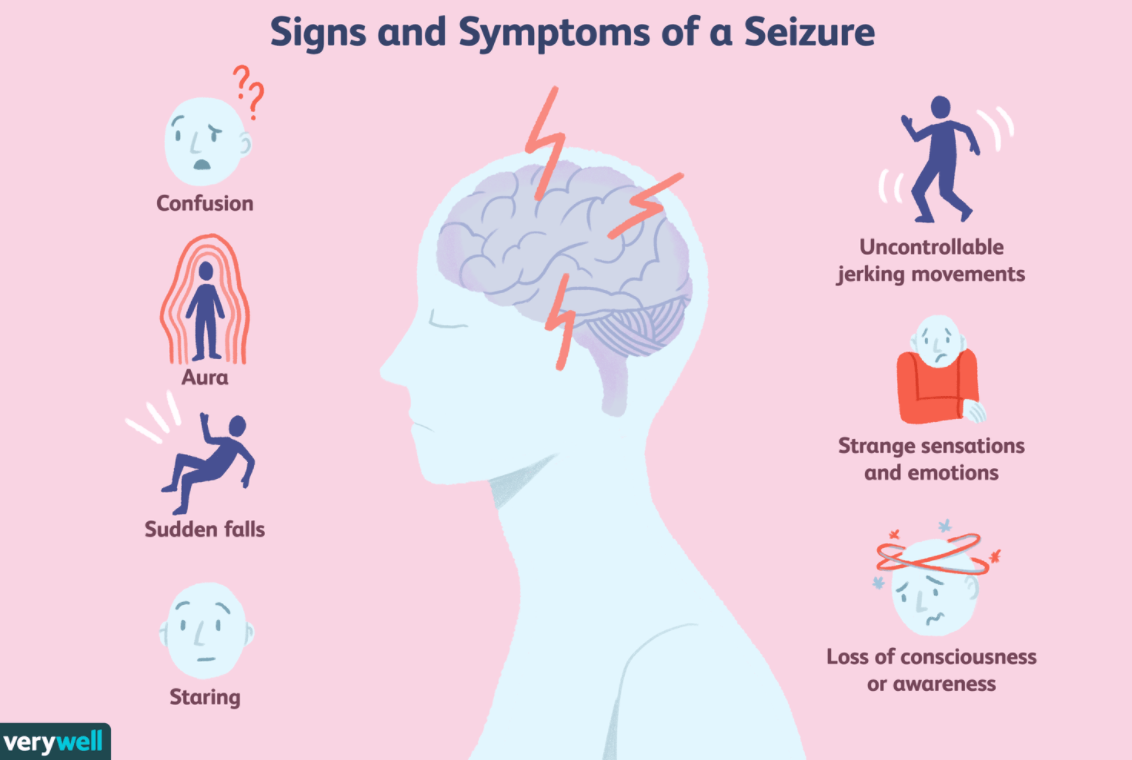 A disorder is defined as an illness that hinders normal physical or mental function and it often encompasses a group of symptoms that may have an undefined underlying specific disease process or treatment. Diseases usually have a defining cause, distinguishing symptoms and treatments. The classification of these terms to specific conditions has been up to debate given the implications it has on societal attitudes, patients themselves and observers like medical professionals. Epilepsy is defined by Epilepsy Canada as a “debilitating neurological disorder” that involves a series of recurrent seizures, which are bursts of uncontrolled electrical impulses between neurons of the brain. This can lead to symptoms such as episodes of involuntary movement (ex: twitches, jerking movements etc.), unconsciousness, and other behavioural and sensory abnormalities. The International League Against Epilepsy (ILAE) has become a global leader by being at the forefront of research pertaining to epilepsy and is responsible for formulating the conceptual definitions of both seizures and epilepsy. Recently, the ILAE recommended a reevaluation of the classification of epilepsy as a disorder into a disease citing that “disorder” implied to the public that epilepsy was a functional and temporary disturbance and did not serve justice to its severity. However, the recommendations of the ILAE have no binding authority and a majority of public health institutions including Health Canada and the Centers for Disease Control (CDC) still classify it as a brain disorder. However, epilepsy’s classification as a disease is more appropriate and has implications that could improve the quality of life of those with epilepsy. Figure 1: Common symptoms associated with seizures which are recurrent with epilepsy First and foremost, delving into elements of the disease concept, the causes of epilepsy remain a contentious topic. Hippocrates in the 5th century challenged the Greek civilization’s pre-existing understanding of epilepsy as a “sacred disease” by offering a specific cause. He argued that the blockage of “phlegm” would result in a discharge that would reach the brain, causing symptoms such as loss of one’s “wits”, partial paralysis, jerking movement, convulsions, etc. This has evolved into our current medical understanding of the causes of epilepsy which can be collectively summarized as disruptions to the brain’s nervous system. More specifically, these causes can be specific brain conditions, head trauma, infectious diseases, prenatal injury, developmental disorders and more. Proponents of those who believe epilepsy is a disorder often cite the fact that in 50% of cases, the cause of epilepsy is unknown and thus the disease classification criteria of a specific cause is lacking. However, emerging research has shown that certain genetic predispositions might make one more susceptible to environmental conditions that trigger seizures and may lead to epilepsy. While many researchers speculate this may be the cause of a large proportion of these cases, current diagnostic techniques are not able to detect if epilepsy is influenced by these factors. Nevertheless, there is a generalized understanding of cause that pertains to the physiological theory of disease as the nervous system disruption is internal. Figure 2: Patient undergoing an EEG which monitors the brain’s electrical activity Additionally, the ILAE has formulated a practical clinical definition of epilepsy that bases its diagnosis on the presence of one of the following 3 conditions: ≥2 unprovoked seizures occurring > 24 h apart, an unprovoked seizure with a ≥60% risk of recurrence or diagnosis of epilepsy. It also considers cases resolved with individuals that reach a certain age if they had an age-dependent condition or if they have been seizure-free for a decade whilst taking no medications for the past 5 years. Thus, despite variability in symptoms, all can be classified as seizures with further diagnosis as epilepsy with a holistic process using the multifaceted definition by the ILAE. Another integral component to disease classification is the patient themselves. Critics of the recommendation posed by the ILAC argue that epilepsy faces a lot of societal stigmatization and the shift would worsen these societal attitudes as diseases have connotations with “infectiousness”, a feature epilepsy is often misunderstood to have. However, this is combated by another misconception in which people underestimate the severity of epilepsy, leading to consequences on patients as they might neglect treatment altogether. It also turns a blind eye to serious forms of epilepsy which can have fatal consequences as seen with SUDEP (Sudden Unexpected Death in Epilepsy). Figure 3: Flowchart representing the onset of a seizure and the various outcomes it might pose
Inevitably, some with severe cases of epilepsy may not be able to be treated. While roughly 70% of those diagnosed with epilepsy can live seizure-free if treated with affordable antiepileptic drugs, 70% of patients don’t receive treatment. This has been coined as the epilepsy treatment gap and is common in many developing countries where physicians lack the training to properly recognize, diagnose, and treat epilepsy. Thus, more accurately labelling the condition as a disease has major implications on patients and can work to improve its prognosis. Disease classification is not only warranted by the fact that specific treatment options like anticonvulsant drugs exist, but it would also result in health policymakers and workers recognizing the severity of epilepsy and work to improve treatment accessibility. Ultimately, the classification of epilepsy as a disease has implications for stakeholders which would allow for the enactment of measures to expand care and treatment, and protect the human rights of patients with epilepsy.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Categories |


 RSS Feed
RSS Feed