|
by Greg Eriksen What is Artificial Intelligence?
Have you ever wondered how self-driving cars work or how Google Home replies to you as if it were human? The answer is artificial intelligence (AI). AI explains the ability for a machine to process information and simulate cognitive functions in response. Through mechanisms such as neural networks and deep learning, a machine can be trained to learn through experience. Consequently, AI machines are able to adjust to new inputs and come up with an appropriate response or action.This ability to accommodate new information helps to explain why self-driving cars don’t shoot off to the side with every bend in the road! What is a Neural Network? One of the primary systems artificial intelligence machines use are called neural networks. A neural network is a computer system that is inspired by the biological inner workings of the human brain. These networks are composed by a series of layers starting at what is known as the input layer. For each input, the system can dynamically analyze the data, which subsequently fires down different pathways of the neural network. The input continuously passes down the layers of the network, with each layer becoming more detailed. Through this filtering process, the system eventually is able to recognize the input and produces an appropriate output or response. What does AI have to do with medicine? Other than being able to sleep while a self-driving car takes you to work, there are plenty of other potential applications for artificial intelligence that are likely more useful! A major area that AI can improve is the analysis of big data, especially in the context of medicine. Big data is data so voluminous that traditional processing mechanisms cannot efficiently analyse it. Using AI technology, big data analytics can examine large amounts of data to uncover hidden patterns and insights in an extremely time efficient manner. In medicine, there are many fields that contain large amounts of data stored deep within online files. These include the millions of images in radiology to the millions of chemical compounds created in drug analysis. With the ever-growing database in medicine, AI machines can access this and run problem solving algorithms in a process that would take humans much longer. In recent development, an artificial intelligence company known as Atomwise has developed a supercomputer which is able to analyse big data more efficiently than ever before. The supercomputer known as AtomNet is particularly used for pharmaceutical analytics. AtomNet is the first structure-based AI system that can predict the biological activity of small molecules used for drug discovery applications. Consequently, the company is able to analyze millions of theoretical molecules without wasting any materials. One of Atomwise’s biggest discoveries came from their research on the Ebola virus. Once the structure of the Ebola virus was found, it was designed on the AtomNet supercomputer. Following this, millions of simulations took place analyzing the different effects of molecules on the virus. In what would have taken traditional analytical processes months, the AtomNet AI system found two potential Ebola fighting treatments in less than one day! The fundamental principle in biology that AtomNet exploits is that structure is largely associated with function. Therefore, the ability to determine where chemical bonding can take place is essential for the discovery of new drugs, and so AtomNet uses a convolutional neural network system that incorporates structural information in its analysis. By doing so, the system can assess how different molecular structures chemically fit together. In similar research to the Ebola virus, AtomNet investigated almost 82 million molecules and eventually discovered a protein-protein inhibitor for a treatment of the autoimmune disease multiple sclerosis! Pharmaceutical analytics is not the only medical field that AI can improve. An AI platform known as Arterys has been developed to assist radiologists in analyzing various medical images! Furthermore, another company known as 3Scan has created a system to efficiently analyze tissue pathology. Perhaps the most exciting partnership with AI technology is with the gene-editing CRISPR CAS-9 system. In short, this system is derived from a bacterial immune response against viruses. The CRISPR CAS-9 complex is able to take the genetic information of a virus and alternatively code for the destruction of that specific virus. With the new advances in genome editing, the CRISPR system can potentially synthesise any DNA molecule. One of the only barriers affecting its prosperity is the problem of off-target effects. To test these potential effects without stepping over ethical boundaries, Microsoft wants to turn to AI technology! The partnership between AI and genome editing may soon revolutionise disease prevention. Artificial Intelligence is making a very strong case for its influence in the medical world. With its major advances in pharmaceuticals, radiology, and genome editing it is paving a very promising future. Although self-driving cars may be awesome, a disease-free world sounds a whole lot better.
0 Comments
by Lauren Lin Huntington’s disease (HD) is a fatal neurodegenerative disease that has symptoms such as chorea (jerky, involuntary movements), loss of coordination, and difficulties with walking, talking, swallowing, focusing, recalling memories, and making decisions. People with HD may also experience increased anxiety, depression, aggression, and impulse control issues. As a neurodegenerative disease, the symptoms begin with subtle issues associated with the previously mentioned symptoms and become more severe over time.
HD is one of the few neurodegenerative diseases that has a clear genetic component. It was identified in 1993 that HD is caused by a mutation in the gene found on chromosome 4 that codes for the huntingtin protein (the Htt gene). Although CAG repeats are found in healthy individuals, individuals with HD have very high numbers of CAG repeats in the Htt gene, and more repeats are associated with more serious manifestations of the disease. The huntingtin gene is dominant, meaning that individuals only need one copy of it from their mother or father to have HD. Therefore, children of parents with HD have a 50% chance of inheriting the disease. Symptoms usually appear between the ages of 35 to 55, but individuals may have symptoms starting before 20 (called Juvenile HD) or in late adulthood (Late Onset HD). The function of the huntingtin protein in healthy individuals is still unclear, but the protein seems to play a role in the function of nerve cells since huntingtin appears to interact with proteins that only exist in the brain. The mutated huntingtin gene leads to abnormal aggregates of huntingtin protein fragments in the brain called neuronal inclusions. The basal ganglia, a brain area that is involved in movement coordination, seems to be the most affected by neuronal inclusions. However, the cerebral cortex, which plays a role in cognitive processes like attention, is also vulnerable to the effects of the huntingtin protein. The symptoms related to the cerebral cortex (i.e. cognitive difficulties) show up later than motor difficulties, which are associated with effects of the abnormal huntingtin protein on the basal ganglia. Currently, there are no drugs that can prevent or slow down the progression of Huntington's disease, but drugs are given to people with HD to help manage their symptoms. For example, some antipsychotic drugs such as haloperidol may be given to patients with HD to help with hallucinations (which sometimes individuals with HD experience), violent outbursts, and chorea. Antidepressant and anxiolytic (anti-anxiety) drugs are also sometimes given to help with the psychiatric symptoms that individuals with HD may have. However, many researchers are investigating new possible treatments for Huntington’s Disease, and a new gene-silencing treatment has been found to have potential in treating HD. A new drug called Ionix-HTTRx is an antisense drug that contains part of a strand of synthetic oligonucleotides that selectively binds to messenger RNA (mRNA) to block translation of all huntingtin protein. The drug is injected into the fluid around the spinal cord, which is then carried to the brain in the cerebrospinal fluid. This month, Ionix Pharmaceuticals reported their findings from a phase 1 trial that included 46 patients aged 25 to 65 from Canada and Europe. The study was 13 weeks long, during which participants were assigned randomly to be injected with one of five possible dosages of IONIS-HTTRx or a placebo. One injection was given each month, and at the end of the study, the participants who received the highest two doses of IONIS-HTTRx had about a 40% reduction in mutant huntingtin (mHTT) levels in their cerebral spinal fluid. The researchers predict that the decreases in mHTT in the cerebral spinal fluid correspond to a 55-85% reduction of mHTT levels in the brain cortex, which may lead to clinically significant results. However, more research trials need to be done with more patients and for longer periods of time to provide a better understanding of whether the drug is truly effective in reducing the levels of huntingtin protein in the brain and helping with HD symptoms. There are plans to conduct more trials beginning later in 2018 or early 2019. Since only one research trial has been done with Ionix-HTTRx and the trial had a very small sample and lasted for a short time, researchers and healthcare professionals do not have enough evidence to support the effectiveness of the drug. That being said, the potential for a drug to decrease the amount of harmful huntingtin protein fragments in the brain brings with it a lot of optimism and hope that we may be able to better treat Huntington’s disease. by Amy Haddlesey 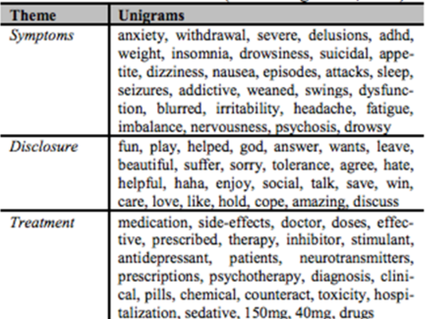 Depression is a mental disorder that is estimated to affect more than 300 million people worldwide. Major Depressive Disorder (MDD) is one of the most commonly diagnosed depressive disorders. MDD is often characterized by having at least 5 of 9 symptoms specified in the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V), with at least one of the symptoms being depressed mood or the loss of interest or pleasure. Other symptoms may include but are not limited to: sleep difficulties, fatigue or loss of energy, reduced ability to concentrate, feelings of worthlessness, and psychomotor agitation or retardation. As a highly prevalent mental illness, it is becoming increasingly important to create new, innovative ways to detect and help depression. In a study done by Microsoft Research, researchers looked into using social media behaviour as a way to infer the behaviours related to depression, with the intention of providing an accessible framework for early detection and diagnosis. The social media platform used in this particular study was Twitter. As a setting for the expression of many significant aspects of behaviour such as a person’s thoughts, mood, activities, and socialization patterns, Twitter provides a wealth of easily accessible knowledge about a person’s emotional condition over time without being intrusive into participants’ lives. In the past, web activity patterns and online behaviour on Facebook have also been studied in relation to mental disorders. For example, researchers have examined trends in Facebook status updates that are associated with depressive symptoms. Using crowdsourcing, the study compiled several hundred Twitter users who participated by completing a CES-D (Centre for Epidemiologic Studies Depression Scale) screening test, Beck Depression Inventory, and an additional survey aimed at gaining depression history and demographic information. A CES-D is a 20-item self-report scale used to measure depressive symptoms. After completing the questionnaires, users could opt in to share Twitter usernames if they had a public profile, under the assumption that their profile could then be mined and analyzed anonymously by computerized programs. Within the study, data or Twitter posts were collected over a yearlong duration from individuals who had given their consent and who had either been diagnosed with depression previously or who had no history of depression. For those who had depression, Twitter data from one year leading up to their diagnosis was collected. For people who did not have depression, Twitter data was collected for the duration of a year ending with the date the survey was completed. In total, 476 users were used within the study. Data from individuals who had depression were used to create a gold standard for the changes in activity on Twitter preceding diagnosis. The behavioural patterns on Twitter of individuals who had depression included: · Posting patterns shifting towards later at night · Decrease in engagement · Higher expression of negative affect · Lower activation · Higher presence of first-person pronouns · Higher use of depression terms · Higher use of words associated with symptoms (Figure 1) · Higher disclosure of feelings and seeking social support · Larger discussion of therapy and treatment Overall, there is a marked increase in certain behaviours and decrease in others before diagnosis that suggests that there may be a shift in behaviour on Twitter leading up to the onset of a depressive episode. By developing this gold standard using data from the depressed group, the study was able to build a statistical classifier that provides an estimate of the risk of depression. In making this prediction, the trend of behavioural change and the degree of the behavioural change the one-year period were both important in identifying behaviour related to depressive symptoms. The study reported that out of their developed models, their best performing model has a 70% accuracy rating for prediction as well as a precision of 0.74. Therefore, the model seems to be able to estimate the risk of depression at an above-chance level, and the model is able to make these estimates relatively consistently. The hopes for this study and moving forward within this area is that the prediction process could aid in identifying behaviour associated with depressive episodes, increase early detection, and lead to having a better support system in place by the time a mental health-related issue presents. Figure 1. Categorization of words into those related to symptoms, disclosure, and treatment. by Jenna Finley We’ve all heard someone say at some point: “I think I’m getting sick so I’ll just take a ton of vitamin C and it’ll be fine.” The idea that a dose of vitamin C will keep you from getting the flu (or at least stop the illness from lingering) is one of the most common home remedies nowadays, and the reason vitamin C tablets fly off the shelves right around the beginning of cold and flu season. However, does this home remedy actually help?
Short answer: we’re not sure. Vitamin C began to be thought of as an important guardian of health in the 1970s when prominent doctors began recommending daily doses as a way for people to lead longer, healthier lives. But it wasn’t until the 1990s that vitamin C began to be more widely touted as a common cold prevention method. Drugs containing vitamin C began popping up on shelves claiming to be common cold cures, the most prominent of which was called Airborne. Since its release, the drug has been the subject of multiple lawsuits over the unsubstantiated claims made involving the “cold busting” power of vitamin C and yet has still inspired dozens of new ‘cold preventing’ vitamin C supplements. As far as research goes, very little support has been found for the idea that taking vitamin C will help prevent an illness, at least for the general public. If you’re an extremely active person who takes a dose of 250-1000mg of vitamin C every single day, then you could reduce your cold incidence by half! Great news for Olympic athletes and marathon runners, but for the rest of us, washing our hands regularly would be more helpful. The possibility of shortening the length of a cold and reducing its symptoms is where the research gets more interesting, though not in the way you might expect. The research findings are also a lot more conflicted in this area. While some studies suggest that vitamin C can reduce symptoms as much as 85%, others say the supplementation makes no difference. The most popular and cited study says that vitamin C can make a difference, but only if a 200mg vitamin C supplement is taken every single day - not just the days you’re feeling sick or the days leading up to a cold. I don’t think a lot of us can say that we meet that condition, but even if we did, the benefits aren’t too exciting. On average, this regime leads to only one less day of illness. Taking a massive amount of vitamin C at once (megadosing) is another common method people use in the hopes that they’ll finally be free of that persistent cold. While some research seems to agree with this treatment, there is yet another caveat. The dose necessary to have a chance at relieving your illness would need to be as high as 8000mg/day, which can cause a whole host of problems. In the end, the 1000mg tablets your roommate is eating like candy around exam season might be doing them more harm than good, as too much vitamin C can make you a lot sicker, resulting in symptoms like vomiting, abdominal pain, and diarrhea. Therefore, we can’t conclusively say that vitamin C supplementation helps, but we do know that it can hurt. Most nutritionists recommend getting your daily needed vitamin C from your meals and forgoing a supplement all together. Doses over 400mg are excreted from the body and can result in you (literally) flushing your money down the toilet. At the end of the day, if you’re still convinced a few vitamin C tablets will help you stave off the dreaded common cold for another day, go ahead and take them, but be careful. No one wants to suffer any more than they have to during exam season. |
Categories |

 RSS Feed
RSS Feed